Are you aware of your blood pressure while at work?
Even those who regularly measure their blood pressure at home may not do so during work hours, especially if they feel nothing out of the ordinary. Nowadays, with automatic blood pressure monitors installed in workplaces, and portable devices that can measure both blood pressure and electrocardiograms (ECGs), it’s technically possible to monitor some vital signs even while on the job. However, the reality is that during work, many find themselves too occupied to spare a moment for such health checks. Some may plan to measure their blood pressure after returning home, but monitoring vitals like blood pressure is particularly crucial in the office environment. Let’s delve into why.
The Necessity of Health Monitoring in the Office Regardless of Age

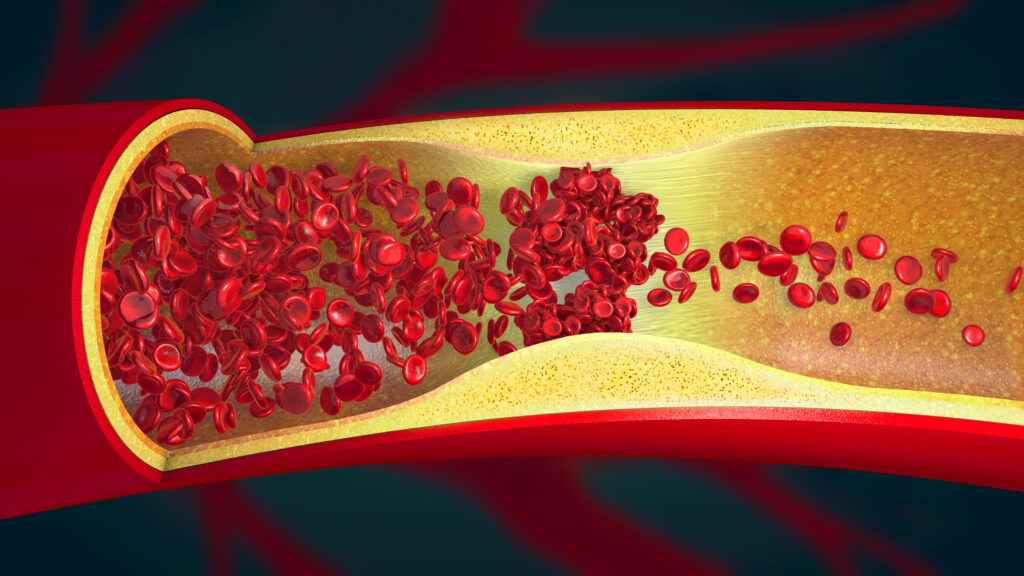
High blood pressure during work is an invisible risk factor for cardiovascular diseases
Even if one’s blood pressure is normal or slightly elevated while resting at home, it can rise during work hours. This condition is known as “masked hypertension.” High blood pressure at work can affect the blood vessels and cause as much, if not more, damage to the brain, heart, and kidneys as consistently high blood pressure does, increasing the risk of cardiovascular diseases. This underscores the importance of monitoring vitals, including blood pressure, during work hours.
High Blood Pressure: Not Just an Issue for the Elderly
This risk applies to all workers, not just older adults. In Japan, 1 in 6 men in their 30s and 1 in 4 men in their 40s have been diagnosed with hypertension (according to the National Health and Nutrition Survey, 2018). There are cases where individuals in their 30s and 40s, who have been told they have “slightly high blood pressure” during health examinations, suddenly suffer from strokes or myocardial infarctions and are rushed to the hospital in an ambulance. The younger the individual, the more likely they are to overlook their health issues.
The Importance of Continuous Health Monitoring from Home to Commute to Office
Heart attacks and strokes tend to occur in the morning and evening
There are specific times when the risk of heart and brain attacks is higher, often in the morning and evening. This means that monitoring is crucial not just at home but also during commute times and work hours. Let’s look at when heart attacks, and strokes are most likely to happen for a clearer understanding of the necessity for continuous monitoring.
For more details on car health monitoring, visit FROM AUTOMOBILES TO HEALTH HUBS: THE FUTURE OF CAR HEALTH MONITORING
Myocardial Infarction
Myocardial infarctions tend to occur more frequently in the morning and evening. Specifically, the peak time for heart attacks is between 8 a.m. and 12 p.m., especially around 10 a.m. This indicates that the risk is higher both during the commute and shortly after arriving at work. The cause is believed to be the rapid increase in blood pressure in the morning.
Cerebral infarction
Cerebral infarctions are more likely to occur from early morning to mid-morning. According to data published in 2018 by the National Cerebral and Cardiovascular Center in Japan and presented in the Circulation Journal of the Japanese Circulation Society, the most critical time for strokes is within two hours after waking up from sleep. This time frame is associated with a sudden rise in blood pressure and increased blood viscosity due to dehydration. According to a survey by iShare Inc., 59.3% of respondents take less than an hour from waking up to leaving home, with 22.0% taking less than 30 minutes. Considering the average one-way commute time is about 40 minutes, it’s conceivable that the high-risk period for cerebral infarctions overlaps with being at home, commuting, or just after arriving at work.
Cerebral Hemorrhage
Cerebral hemorrhages are particularly likely to occur in the morning and evening. Specifically, the critical times are from 7 a.m. to 10 a.m. and around 5 p.m. These times correspond to when people are preparing to leave home, during the commute, and shortly after arriving at work. The morning risk is attributed to the rapid rise in blood pressure following the overnight drop during sleep, while the evening risk is due to the increase in blood pressure from the day’s activities and the tendency for blood vessels to constrict due to physical and mental stress.
The Best Solution for Continuous Monitoring: Wearable Devices

Given the above, we understand that (1) vital monitoring in the office is necessary regardless of age, and (2) coordinated health monitoring from home to commute to office is essential. Now, let’s discuss the technology that can fulfill these needs. Currently, wearable devices, exemplified by smartwatches, are the most feasible technology for this purpose.
The Need for Continuous Office Health Monitoring
During work, vital signs, including blood pressure, fluctuate depending on the situation—whether one is working at a computer, meeting with clients, or dealing with work-related troubles. The reason for these fluctuations is that the type of stress encountered varies from one scenario to another. Consequently, it becomes necessary to continuously monitor blood pressure throughout the workday to capture these variations accurately. In this respect, wearable devices, such as smartwatches, are superior to stationary monitors. They provide the flexibility and continuity necessary to effectively track vital signs through various work activities.
Ease of Integration from Home to Commute to Office
Wearable devices, simply by being worn, allow for constant health monitoring without being limited by location or time. However, there are moments, such as during bathing or showering, when the device might be removed, which ironically could be when the risk of a heart attack or stroke is highest.
Ideally, Predicting an Episode; Next Best, Detecting the Onset
Reducing Sudden Deaths through Episode Prediction
The ideal scenario is to predict an episode before it occurs. The longer the lead time before an actual episode, the higher the chance of saving a life. If an episode is predicted, work can be stopped immediately, emergency services contacted, and the individual can be taken to the hospital by ambulance. According to the 2022 report from the Fire and Disaster Management Agency of Japan’s Ministry of Internal Affairs and Communications, the average time for an ambulance to arrive on the scene is approximately 9.4 minutes, and the average time to hospital admission is about 42.8 minutes. If it were possible to predict an episode one hour before it occurs, the response to the episode could be perfectly executed. Even if the prediction comes just minutes before an episode, contacting emergency services and taking measures to rest could make a difference.
The Significance of Detecting the Onset of an Episode
Predicting an episode is inherently challenging. As we will explore further, relying solely on wearable devices for prediction is particularly tough. Thus, a more feasible approach may be detecting the onset of heart attacks or strokes using wearable devices, which is more likely to be achievable. When an episode occurs, the individual may notice unusual symptoms but may not understand what’s happening. If others are around, they can contact emergency services, but if the person is alone, they may not be able to do so. In such cases, if a wearable device detects the episode and contacts emergency services, it significantly increases the chance of survival. Hence, the most significant advantage is the ability to make such emergency contacts, especially if the device can also identify the type of medical emergency, facilitating a smoother response from emergency services.
The Potential of Wearable Devices in Detecting the Onset of an Episode
Promising Indicators for Episode Detection
Wearable devices have significantly advanced in their ability to measure a wide range of bodily information. For instance, they can monitor heart rate, blood pressure, electrocardiograms (ECG or EKG), oxygen saturation, respiratory rate, steps and physical activity, sleep patterns, calories burned, skin temperature, and even UV exposure, among others. Among these, the potential to detect sudden changes in the body that could indicate the onset of an episode lies in monitoring heart rate, blood pressure, and electrocardiograms.
- Electrocardiogram Monitoring: Some wearable devices come equipped with the functionality to measure electrocardiograms, detecting abnormalities in the heart’s activity. For example, the onset of acute myocardial infarction is indicated by ST elevation in an ECG. If a wearable device can detect ST elevation, it suggests the possibility of an acute myocardial infarction. However, as other heart conditions can also cause ST elevation, it cannot definitively diagnose a heart attack.
- Blood Pressure Monitoring: High blood pressure is a risk factor for both myocardial infarction and strokes. Some wearable devices support blood pressure monitoring, alerting the user when blood pressure levels are abnormally high. However, during a heart attack or stroke, blood pressure can either rise or fall, so changes in blood pressure alone cannot confirm the onset of an episode. Furthermore, sudden changes in blood pressure could result from various diseases or stress, making it unreliable as the sole indicator of an episode.
- Heart Rate Monitoring: An unusually high or irregular heart rate can be a sign of potential heart-related issues. However, like blood pressure, heart rate can increase or decrease during a myocardial infarction or stroke, making it challenging to deduce the occurrence of an episode based solely on heart rate variability. Additionally, rapid changes in heart rate can be caused by a range of diseases or stress factors, complicating its use as a definitive marker for an episode.
Challenges and Directions for Wearable Device Use in Episode Detection
From this overview, several challenges emerge in using wearable devices for episode detection:
- The increase in blood pressure and heart rate is not specific: Everyday stressors can cause fluctuations in these metrics, meaning that their elevation does not necessarily indicate an episode.
- A significant drop in blood pressure or heart rate signals a serious condition: By the time such changes are detected, the individual may already be in a critical state, underscoring the need for earlier detection.
- The necessity for multimodal information: To accurately identify the occurrence of an episode, it’s insufficient to rely on a single type of vital information. Integrating multiple modalities of data is essential for precise detection.
Enhancing the capability of wearable devices to capture a broader spectrum of bodily information, or integrating additional measurement technologies within environments such as offices, vehicles, and homes, could significantly improve the detection of the onset of medical episodes. This strategy suggests not only expanding what wearable devices can measure but also supplementing them with other monitoring technologies to gather critical data that wearable devices alone may miss.
Can Wearable Devices Predict Episodes Alone?
Why Predicting Episodes is Challenging
Currently, there’s no wearable technology that can predict episodes before they occur. Firstly, changes in blood pressure and heart rate are not specific to cardiovascular episodes. While wearable devices can detect abnormalities such as ST elevation in electrocardiograms, these signs don’t appear until after tissue damage has begun, making prediction difficult. As for strokes, wearable devices that examine brain waves are still in the research phase.
Wearable Devices × Big Data × AI: The Future of Episode Prediction Research
If we can collect long-term measurement data on heart rate, blood pressure, and ECGs from a vast number of users and create a system to report episodes, AI could potentially learn to identify specific changes in these measurements that precede episodes. Academic institutions and technology companies are collaborating to explore ways to monitor health status using wearable devices and identify risks of severe health problems early. Whether this will become a reality remains to be seen, but it’s undoubtedly a crucial direction for research.
Limitations of Wearable Devices
Wearable devices, combined with big data and AI, hold promise, but it’s also essential to recognize the limitations of wearable devices themselves.
- Incomplete ECG Data: Compared to clinical examinations, the ECG data obtained from wearable devices are incomplete.
- Not Always Wearable: The most wearable devices, like smartwatches, can’t always be worn, especially during private moments like bathing or showering, which ironically might be when the risk of an episode is highest. Considering built-in vital monitoring technology in bathrooms could be a direction worth exploring.
- Limited Brain Information: Smartwatches cannot detect brain waves. While hat-type, earphone-type, hairband-type, and headgear-type devices are being developed, it’s unclear if they can be used as regularly as smartwatches.
- Direct Examination of Blood Flow Changes is Not Possible: Cardiovascular episodes involve significant changes in the blood flow to the brain and heart, making blood flow changes a more direct indicator than ECG, heart rate, or blood pressure. Currently, there’s no wearable technology to directly detect these changes in blood flow.
Driving Research Towards More Advanced Sensors Built into Life and Work

Office Equipment with Built-In Sensors: Smart Desks and Chairs, etc.
Our daily lives are surrounded by numerous items, among which, in offices, desks and chairs that come into contact with the human body and computers that people stare at hold promise for health monitoring. By building sensors into these items, it’s possible to obtain more detailed or advanced biometric information than wearable devices can provide. Indeed, research and development into smart chairs that can measure heart rate and respiration rate have been conducted, but so far, they measure the same biometric information that wearable devices do, without surpassing them.
Case Studies in Cars
Ford and Toyota’s Denso have developed technology that can measure ECGs from the driver’s seat and steering wheel, respectively. Chairs with more contact points with the body than a smartwatch can potentially measure more detailed ECGs, possibly offering advantages in detecting ECG abnormalities caused by myocardial infarction.
For more details, visit FROM AUTOMOBILES TO HEALTH HUBS: THE FUTURE OF CAR HEALTH MONITORING
Investing in Sensor Development to Monitor the Blood Vessels and Blood Flow of the Heart and Brain
Premonitory Signs Exist Before an Episode
As mentioned earlier, ECG abnormalities do not appear until myocardial necrosis occurs in the case of myocardial infarction. However, it’s known that there are precursors to myocardial infarction and strokes, indicating that some abnormalities do occur within the body before an episode occurs. To predict episodes, we should focus on developing sensing modalities that can capture these changes.
Approaching the Essence of Cardiovascular Episode Prediction: Monitoring the Blood Vessels and Blood Flow of the Heart and Brain
For example, technologies that can monitor changes in blood flow and the condition (spasm or narrowing) of the coronary arteries in real time have a high potential for predicting episodes of myocardial infarction. Similarly, for predicting strokes, monitoring the cerebral and carotid arteries is considered effective. In hospitals, catheter angiography and MR and CT angiography are used to capture changes in blood flow and the condition of vessels, but these methods require contrast agents and are invasive. Non-invasive alternatives offer limited information. Moreover, these tests require large equipment and specialized rooms due to their use of magnetic fields or radiation. On the other hand, to monitor changes in vessels and blood flow daily in offices, vehicles, and homes, the technology must be non-invasive, small, and usable in everyday spaces.
Wearable devices have enabled continuous monitoring at the expense of completeness in measurement. Similarly, research and development for vascular blood flow and structure sensors should also proceed with a focus on being non-invasive, compact, and usable in everyday spaces, even if it means sacrificing the completeness of measurements
For more details, visit MONITORING BLOOD VESSELS: REAL INDICATORS OF YOUR HEALTH
The Future of Healthcare Created by (Wearable + Built-in Sensors) × Big Data × AI

Wearable technology is unparalleled in terms of continuous monitoring, but due to the necessity of wearing the device comfortably on the body, there are limitations in size and the body surface areas where devices can be placed, leading to restrictions on what can be measured and partial measurements. Complementing this are sensors that can be built into living spaces. While built-in sensors may not match the continuity of measurement offered by wearable devices, they have a higher potential for capturing more sophisticated health information. By integrating wearable devices with built-in sensors, collecting big data, and using AI to aggregate and analyze the data, we foster strong hope for a future where we can predict life-threatening emergencies on an hourly and daily basis. Here’s to saving as many lives as possible from the brink of crisis.
For more details, visit [PURSUING TECHNOLOGY TO CREATE A WORLD WHERE EVERYONE’S MENTAL AND PHYSICAL HEALTH IS MONITORED: THE WORLD WATCHED OVER BY MOTHER AI]
