The Future of Medical Care: Home Monitoring

Our bodies change every day, yet most of us only visit the clinic once a month at most. This means that relying solely on clinic tests and examinations may not fully capture these daily changes in our bodies. For this reason, devices that allow self-measurement of blood pressure and blood sugar levels have been developed, and patients with high blood pressure or diabetes are recommended to monitor these levels daily at home. This practice of daily home monitoring helps to understand the daily changes in our bodies and enables optimal treatment – that is, the most effective treatment without waste.
While home monitoring is recognized as beneficial, its implementation for age-related macular degeneration (AMD) remains a challenge. I have co-developed a tabletop Optical Coherence Tomography (OCT) device that allows self-imaging at home, in collaboration with Medimaging Integrated Solution (MiiS), a medical device manufacturer in Taiwan. This is the ‘Home OCT.’ Furthermore, the image data obtained from Home OCT is automatically transmitted to the cloud via a smartphone, and analyzed by AI. This communication feature of the OCT was developed in collaboration with Mr. Kobayashi, former head of OCT development at NIDEK Co., Ltd. This system, the ‘Home OCT Monitoring System,’ is what I believe to be a significant advancement in optimizing treatment for age-related macular degeneration. I would like to discuss the concept of the Home OCT Monitoring System and how it can help in the treatment of AMD. This will involve some technical discussion, starting with a brief explanation of OCT and AMD. If you are already familiar with these, feel free to skip ahead.
What is OCT?
OCT, or Optical Coherence Tomography, is a medical device used to non-invasively obtain cross-sectional images of the retina. It uses light to detail the various layers of the retina, aiding ophthalmologists in diagnosing retinal diseases. OCT has become an indispensable test in the diagnosis and treatment of age-related macular degeneration. Initially, OCT had a significant drawback in that the time-domain method used for imaging was slow. However, the second-generation spectral-domain method was commercialized, significantly speeding up imaging and making it suitable for routine clinical practice. During my time at Kyoto University, I participated in the development of a spectral-domain OCT prototype in collaboration with Dr. Yoshiaki Yasuno, a lecturer (now professor) at Tsukuba University, and Topcon Corporation. This led to the launch of the world’s first commercial spectral-domain OCT device. I have authored 104 English-language papers on OCT. This experience and track record have given me deep insights into how OCT can be utilized in ophthalmology.
What is Age-Related Macular Degeneration (AMD)?

In age-related macular degeneration, the macula, located at the center of the retina and responsible for vision, is affected, causing the central field of vision to become unclear. Commonly seen in older adults, it impacts activities requiring vision, such as reading and driving. As such, in today’s internet-dominated society, it increasingly leads to difficulties in daily life. It is the leading cause of blindness in Western countries and is rapidly increasing in Japan as well, alongside the Westernization of dietary habits.
I know several people with age-related macular degeneration. While walking is not a problem for them, shopping becomes a challenge as they can’t see the prices and product details like before. Many have stopped driving, making life more difficult. Moreover, they struggle with activities they used to enjoy, like reading, and have trouble seeing the faces of their grandchildren and family clearly, often losing the joys of daily life and becoming mentally distressed. This condition is not only a significant psychological burden for the patients but also for their families.
Japanese dietary culture and age-related macular degeneration prevention: learning from tradition
Rapidly Progressing Exudative AMD and Its Treatment: Anti-VEGF Therapy
Age-related macular degeneration comes in two forms: ‘exudative,’ which progresses rapidly, and ‘atrophic,’ which progresses very slowly. In Japan, the exudative form is more common. In exudative AMD, new, abnormal blood vessels from the choroid, a layer of blood vessels meant to protect the macula, grow under the retina where they shouldn’t be. This leads to the leakage of blood components and fluid accumulation under the retina (subretinal fluid or SRF), swelling of the macula (cystoid macular edema or CME), and even bleeding, resulting in the loss of central vision.
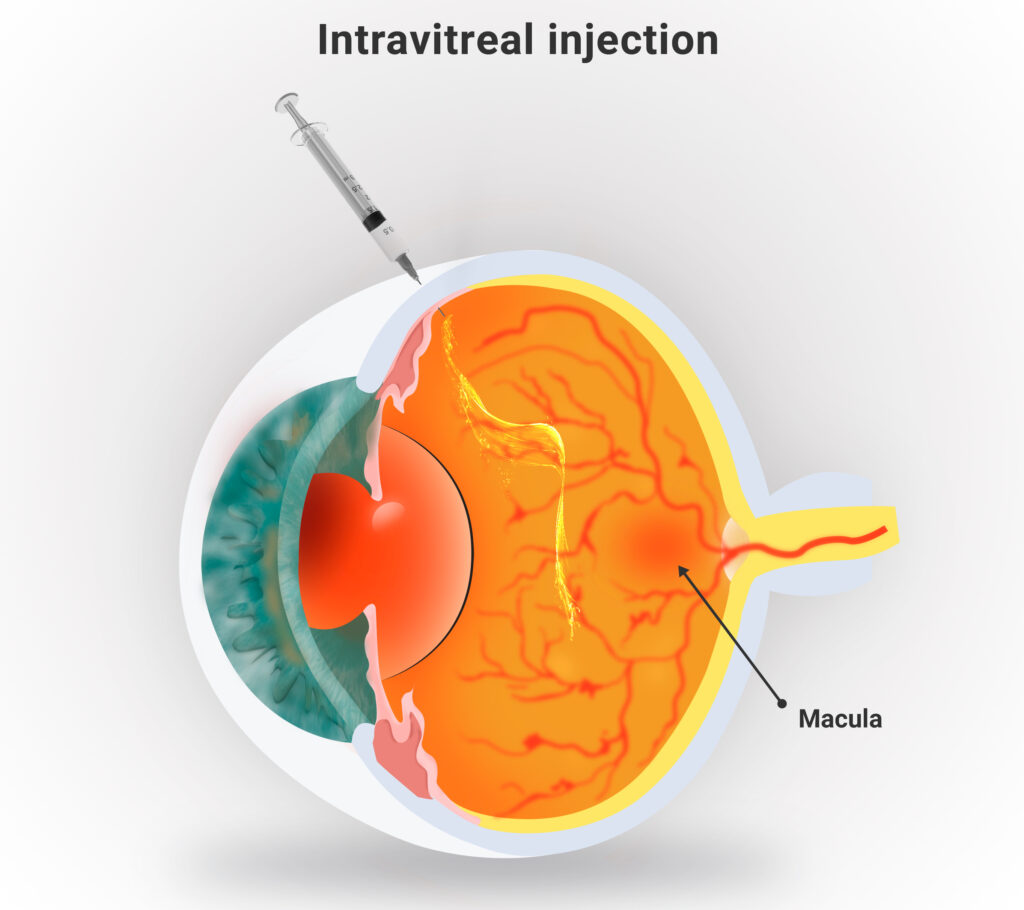
The current first-line treatment for exudative AMD is intravitreal injection of anti-VEGF antibodies. VEGF, a vascular endothelial growth factor, has two functions: promoting new blood vessel growth and increasing vascular permeability. While essential for vascular health, in conditions like AMD, it is overproduced, leading to the formation of new blood vessels and making them leaky, causing SRF and CME. Injecting anti-VEGF antibodies into the vitreous of the eye inhibits the growth of these new blood vessels and stops the leakage. Consequently, the blood components accumulated under or within the retina are quickly absorbed, improving vision.
Challenges in Treating Age-Related Macular Degeneration: Recurrence and Endless Injection Treatments
While anti-VEGF antibody therapy is effective, its effects are not long-lasting, necessitating repeated injections, which poses a significant problem. The effectiveness of a single injection varies depending on the type of medication and the condition of the eye, typically lasting about 1-3 months. Therefore, patients initially receive monthly injections for three months, followed by injections as needed based on recurrence. However, anti-VEGF therapy cannot completely eliminate choroidal neovascularization; the root part remains. If the injections are stopped, recurrence occurs. As a result, many patients undergo numerous injections over many years, presenting a substantial economic and effort burden. The minimal treatment is desired for this reason.
An additional problem is that, despite continuous treatment efforts, some patients experience gradual vision loss. One reason for this is recurrence. The timing of recurrence is unpredictable. The current basic treatment protocol involves monthly examinations and OCT tests. If SRF or CME recurrence is detected, an anti-VEGF antibody injection is administered. However, this approach inevitably results in a significant time lag between recurrence and injection, potentially damaging the macular neurons. A method of extending the injection interval to every half month was devised, but this risks over-treatment. Ideally, an injection should be administered as soon as signs of recurrence are detected. To achieve this, daily OCT testing is necessary. However, it is not feasible for patients to visit the clinic every day. Hence, the need for a Home OCT that allows self-imaging.
The Concept of Home OCT Monitoring for Managing Age-Related Macular Degeneration
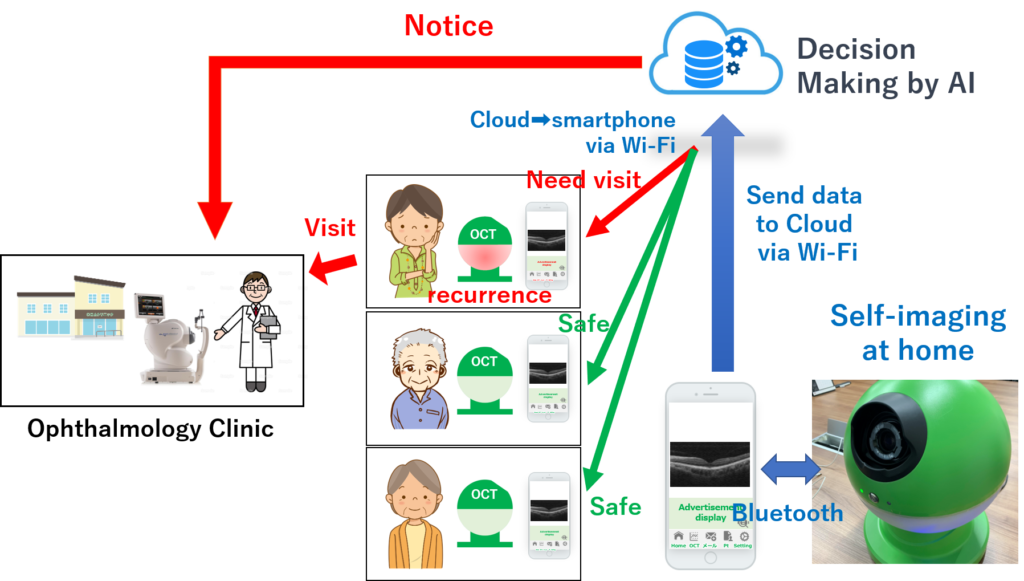
The outline of our Home OCT-based system for detecting the recurrence of age-related macular degeneration is as follows: Patients use the Home OCT, placed at their home or workplace, to take daily self-images. It may not be necessary immediately after an injection, but starting about 20 days post-injection, daily imaging is recommended. Each time an image is captured, the data is instantly sent to the cloud via a smartphone, and AI assesses for any signs of recurrence, immediately informing the patient of the results. A ‘no recurrence’ result allows the patient to continue their day as usual, whereas a ‘recurrence detected’ result prompts an immediate visit to the ophthalmology clinic for treatment. The data and AI results are also simultaneously shared with the affiliated ophthalmology clinic.
Challenges in Developing a Home OCT System for Age-Related Macular Degeneration Management
To develop a Home OCT system for managing age-related macular degeneration, we had to overcome the following challenges:
Self-Imaging: In a home setting, there are no medical technicians, and spouses, often elderly themselves, cannot be relied upon for assistance. Some patients live alone. Easy self-imaging was therefore essential.
Miniaturization: OCT devices used in clinics vary in size but are generally too large for home use. A size comparable to a microwave oven would be more suitable for a home device.
Cost: Clinic-based OCT devices, depending on the model, are expensive, often costing around ten million yen, making them unaffordable for home use. Our goal was to reduce the cost to around 300,000 yen, comparable to household appliances.
Real-Time Decision Making: Storing OCT test results to show them only during a monthly eye clinic visit would be meaningless. It’s crucial to make an immediate decision about the necessity of a re-injection based on each test.
Our Solutions
Self-Imaging
In standard OCT, patients first place their face on a chin rest and fixate their eyes on a target light, allowing the technician to position the test light and capture images. Proper alignment is crucial for high-quality images. Moreover, patients with age-related macular degeneration may have difficulty seeing the fixation light due to their central vision loss. To enable self-imaging with OCT, both medical insight and technical innovation were necessary. Thanks to the superior technology from MiiS for self-imaging, we were successful in developing a self-imaging OCT.
Miniaturization and Cost Reduction
This is a matter of product philosophy. To put it simply, it’s like deciding whether to make a Lexus or a Corolla. Traditional OCT devices are, of course, designed with clinic-based physicians in mind, equipped with many features and capable of handling various diseases. However, our goal was specifically to detect the recurrence of age-related macular degeneration. By eliminating all functions unnecessary for this purpose, we could achieve both miniaturization and cost reduction. As an aside, since the device would be placed at home, we also wanted it to be aesthetically pleasing and not just look like a medical device. We estimated that mass production could bring the cost down to around 300,000 yen.
Real-Time Decision Making
This is the crux of the Home OCT Monitoring technology. First, the digital image data captured by the OCT is transmitted to the smartphone via Bluetooth and then sent from the smartphone to the cloud via Wi-Fi. The data sent to the cloud are not only stored but also immediately analyzed by AI for signs of recurrence. The results of this analysis are then sent back to the smartphone via Wi-Fi, indicating either ‘no recurrence’ or ‘recurrence detected: re-injection required.’ Considering the possibility that some patients may not be able to read the smartphone’s text, we also enabled recognition through color display. For example, the smartphone screen could display blue for ‘no recurrence’ and red for ‘recurrence detected: re-injection required.’ Alternatively, these colors could be displayed on the OCT device itself via Bluetooth. This entire process of testing ➡ decision-making ➡ notification occurs within a few minutes.
Seeking Global Development Partners
Although there are a few companies worldwide that have succeeded in developing Home OCT, to my knowledge, none are specialized in a service that informs patients of the timing for their medical appointments using AI, as we do. Nor are there companies aiming for cost reduction like us. This is because, unlike other companies, we do not consider the OCT hardware as our primary source of revenue; rather, our business model focuses on the service of informing patients about their appointment timing. We have completed the development of our prototype and are currently seeking partners for business expansion.
The Convergence of AI, Networking, and Sensing Technologies
The use of OCT technology, traditionally a diagnostic tool in clinics, transformed into a home monitoring system by adding AI and network technology, serves as an excellent example. Around the world, various technologies exist to protect people’s health. The medical device industry is at a point where it needs to shift from a clinic-based or physician-based mindset to a patient-based approach.
